Julia Hathaway (Environmental Science)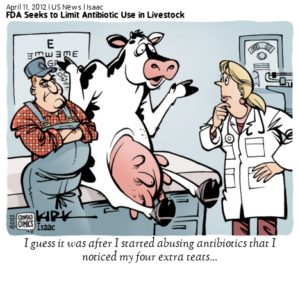
Lauren Rae (Animal Science)
Evan Lunetta (Forestry)4323
Have you ever taken a bite out of your favorite food or sipped tap water and thought to yourself, “is this going to make me sick?” Perhaps poured an ice-cold glass of water from the sink, gulped a refreshing sip and wondered if it could kill you? Most people would say no. Unfortunately, in just a short-while, this will no longer be a question we can answer no too. The New York Times posted an article just a few days ago titled, “Fear, Then Skepticism, Over Antibiotic-Resistant Genes in Beijing Smog,” reporting smog over China containing antibiotic resistant genes. The Times described the smog spreading through the city, “like pathogens in a pandemic disaster movie” (Tatlow, 2016, para. 5). Chinese citizens are scared, especially for their children. The article quoted a young Chinese actress saying she wanted to pick up her 11-month-old daughter and run away because the smog would make it easier for her daughter to become sick (Tatlow, 2016). The most alarming part is the Chinese are so used to their disease ridden air, the antibiotic resistant contaminated air is only of mild concern given their other current environmental hazards (Tatlow, 2016). As alarming as that truth is, the Chinese are not the only people impacted by antibiotic resistant bacteria. The Center for Disease Control stated that antibiotic resistant bacteria now affects 2 million Americans each year and results in 23,000 deaths (CDC, 2016, para. 2). The CDC estimates by 2050 antibiotic resistance will have killed 10 million people worldwide (Walsh, 2014, para. 1). Imagine, in just a few more decades as human population reaches an all time high, death by antibiotic resistant bacteria will become even more common than death by cancer and unlike cancer, there is no hope of treatment (Walsh, 2014).
Everyone needs food to survive, and as population is estimated to almost double in the United States alone by 2050, it is estimated that in 4 years our countries consumption of meats will also double, in turn leading to an exponentially growing livestock industry (Pew Research Center, 2008). In order to accommodate growing meat demands, livestock production has become increasingly more industrialized (Brooks, 2011). The use of antibiotics in livestock has become a common management practice (Brooks, 2011). They are used to control bacterial pathogens that cause disease and especially as growth promoters to produce marketable meat quicker (Brooks, 2011). They are effective in some situations, however they pose significant risks (Brooks, 2011). The most important issue is the transport of antibiotics and how they come in contact with humans. Antibiotic contaminated groundwater and surface water is threatening the health of humans and in order to prevent this problem we propose to ban the use of antibiotics for non-therapeutic and sub therapeutic purposes, reducing groundwater and surface water contamination.
These antibiotics are authorized for a variety of reasons, around 70% of all antibiotics administered are done so through feed or drinking water for production purposes (Beecher, 2015. para.14). The USDA defines ‘production purposes’ as the use of antibiotics on livestock in barns, dry lots, or houses for growth promotion (USDA, 2015). Unfortunately, non therapeutic treatments are on the rise in the meat industry. As early as the 1940s, researchers discovered that animals fed low levels of antibiotics experienced faster rates of growth and improved feed efficiency (Hays, 1999). Antibiotics lead to growth promotion in livestock by improving energy efficacy of the gut (Antimicrobial Resistance Learning Site, 2011). Livestock play host to many kinds of gut microbes that help break down food (Animal Smart, 2016). Although these microbes are useful in digestion and immune response, they also compete with the animal for nutrients (Animal Smart, 2016). Small doses of antibiotics in animal feed reduce this competition, allowing the animal to convert feed to muscle more quickly causing rapid growth (Animal Smart, 2016). It is the overuse of antibiotics for productive purposes that cause antibiotic resistant bacteria to develop (American Meat Institute, 2016). The meat industry is currently justifying the mass use of antibiotics in livestock to keep up with rising meat demands (Animal Smart, 2016). Other common reasons for antibiotic consumption are to treat or prevent illness, prohibit pain, and stop early signs of illness in livestock (South Dakota State University, 2016). These three methods are all considered therapeutic uses of antibiotics. Merriam-Webster defines therapeutic as the treatment or healing of illness or disease (Merriam-Webster, 2016). Antibiotics used for nontherapeutic purposes are usually administered through mixing with either water or feed (South Dakota State University, 2016). Antibiotics used for production purposes provide an economic appeal because the animals require less feed per unit of growth (Sneeringer, McDonald, Key, Mcbride, & Matthews, 2015).
The rapid emergence of resistant bacteria is occurring worldwide as a result of antibiotic overuse and endangering the the efficacy of antibiotics (Ventola, 2015). In order for resistance to occur, the bacteria must come in contact with the antibiotic, resistance must develop, and then be passed to daughter organisms or other organisms of the same species (Khachatourians, 1998). Resistance specifically develops in 2 ways, by mutations that change the bacteria’s genetic material, or by acquiring resistance from another bacteria (Alliance for the Prudent Use of Antibiotics, 2014). Mutations are rare and occur spontaneously in about one in one million to one in ten million cells (APUA, 2014). Some mutations allow the bacteria to produce chemicals that inactivate antibiotics, some close the points of entry into the cell, and others manufacture pumping mechanisms to pump the antibiotic back outside of the cell (APUA, 2014). Any bacteria that acquire resistance genes has the ability to resist one or more antibiotics (APUA, 2014). Essentially, the mutations give the bacteria a defense against the antibiotics. Bacteria can also pick up resistance from other bacteria through a process called conjugation (APUA, 2014). This process allows bacteria to transfer genetic material, including genes encoding resistance to antibiotics (APUA, 2014). This is the same process that happens in humans, resistance occurs when the bacteria is challenged but not destroyed (American Meat Institute, 2016). Essentially, what doesn’t kill the bacteria only works to make it stronger.
There is an estimated 132 million metric tons of manure produced annually from cattle, swine, and poultry production in the US alone (Dolliver, Kumar, & Gupta, 2007, p.1224). There is 24.6 million pounds of antibiotics used annually in livestock and as much as 75% of antibiotics delivered are not absorbed or used by the animal (Mackie et. al, 2006, p.157). The 75% of antibiotics not absorbed by the animal must exit the body (Mackie et al., 2006). Antibiotic resistant bacteria exit the animal via feces and urine. These contaminated manures are then used for agricultural purposes and eventually end up in groundwater and surface waters as a product of runoff (West, Liggit, Clemans & Francoeur, 2011).
This is of particular concern in Concentrated Animal Feeding Operations or CAFOs. The Environmental Protection Agency defines a ‘CAFO’ as an area that confines an animal for more than 45 days during a growing season in an area that does not produce vegetation and meets certain size thresholds. According to Hribar and Schultz (2010), antibiotics leave the CAFO and “contaminate groundwater and surface water through runoff from land application of manure, leaching from manure that has been improperly spread on land, or through leaks and breaks in storage containment units” (Hribar & Schultz, 2010, p.3). Soil erosion is also a contributing factor to water pollution. If pollutants bond to eroded soils, they can potentially move to nearby watersheds, infecting large bodies of water (EPA, 1998). Antibiotics can persist in soils from a few to several hundred days depending on the type (Dolliver et al., 2007). West et al. (2011) noted that the majority of bacteria found in agricultural soils are commonly found in the guts and feces of warm-blooded animals, suggesting that the bacteria came directly from livestock. Due to the dense populations in CAFOs, antibiotic resistant viruses are easily transported between animals and potentially to surrounding areas (Hribar & Schultz, 2010). In order to determine the exact effects of antibiotic resistant bacteria transport in CAFOs, water quality measurements such as fecal coliform density are often tested (West et al., 2011). They are performed upstream and downstream of CAFOs to determine where concentrations of antibiotic resistant bacteria are at their highest (West et al., 2011). These water quality tests are useful to determine where the majority of antibiotic resistant bacteria end up after leaving a CAFO (West et al., 2001).
Antibiotic contaminated ground and surface waters pose a significant risk to human health. Groundwater contaminated, via runoff, present a threat to drinking water supply (Hribar & Schultz, 2010). The EPA estimates that more than half of the population relies on groundwater for drinking water, and this number increases dramatically in rural areas (EPA, 2004). Bacteria that have become resistant and can no longer be treated with antibiotics, can cause serious health risks in humans, including death (Hribar & Schultz, 2010). Nearly half of the antibiotics administered to animals are also used in humans (Kaufman, 2000). This is concerning as humans are increasingly exposed and infected with antibiotic resistant bacteria from agricultural practices. Since we use the same antibiotics given to livestock, we no longer have a way to kill off the resistant bacteria leaving humans vulnerable to long term infections (Kaufman, 2000). Already, alarming levels of antibiotic resistant bacteria have been found in waters used for drinking and agricultural purposes (Sapkota, Curriero, Gibson, & Schwab, 2007). Groundwater is not the only concern, contaminated groundwater can also impact surface waters. Hribar and Schultz. (2010) explain that, “contaminated groundwater can move laterally and eventually enter surface water such as rivers and and streams” (Hribar & Schultz, 2010, p.4).
Already, alarming levels of antibiotic resistant bacteria have been found in waters used for drinking and agricultural purposes (Sapkota, Curriero, Gibson, & Schwab, 2007). Groundwater is not the only concern, contaminated groundwater can also impact surface waters. Hribar and Schultz. (2010) explain that, “contaminated groundwater can move laterally and eventually enter surface water such as rivers and and streams” (Hribar & Schultz, 2010, p.4).
In order to eliminate this problem, we propose to ban the use of all non-therapeutic and subtherapeutic antibiotics in livestock. Administering only therapeutic antibiotics will constrain bacteria from becoming resistant and infecting surrounding areas. These measures will also drastically reduce the amount of antibiotic resistant bacteria in ground and surface waters thereby, reducing water contamination and the threat to human health. The Food and Drug Administration has approved the use of antibiotics in livestock for over 40 years (Zeller, 2016). The Center for Disease Control reported that time duration of antibiotic treatment therapy, or choice of antibiotic is incorrect in 30% to 50% of cases (Ventola, 2015). The FDA has released 2 documents to promote the judicious use of antibiotics in food animals (FDA, 2015). The documents provide guidance for drug companies to “voluntarily revise the FDA-approved use conditions to remove the use of antibiotics for preventive purposes, add scientifically supported disease treatment control or preventative uses, and change the marketing status from over-the-counter Veterinary Feed Directive for drugs administered through feed in order to provide veterinary oversight or consultation” (FDA, 2015, para. 2). As of now, all of these proposals and implemented regulations are voluntary for farmers due to the F.D.A.’s hope that pharmaceutical companies making the drugs, will work willingly with the F.D.A. to revise the conditions of antibiotic use (U.S. Food and Drug Administration, 2016). The FDA is putting the majority of responsibility on veterinarians to prescribe antibiotics for subtherapeutic and therapeutic uses (FDA, 2015). The FDA stated, “veterinarian practicing judicious use principles would consider relevant factors to determine the risk of a specific bacterial disease and whether it would be appropriate in a particular situation to use medically important antibiotics for prevention purposes” (FDA, 2015, para. 3). These regulations do not assure the overall safety of antibiotic use in livestock, instead it puts the decision into individual hands. “The lack of regulations on antibiotics used for production purposes results in antibiotics that are easily accessible, plentiful, and cheap, which promotes overuse” (Michael, Dominey-Howes, & Labbate, 2014).
CAFOs have specific regulations as well. Right now, CAFOs must have a number of permits in order to dispose of their animal waste and even more permits if their farm resides near fresh water (Environmental Protection Agency, 2016). Farmers must follow the USDA’s standard calling for a 120-day time interval before the untreated manure could be used for soil in order to ensure any remaining antibiotics are nonfunctioning (Beecher, 2015). These regulations are not enough to stop the build up of antibiotic resistant bacteria in our water systems. This is why we propose eliminating the use of non-therapeutic antibiotics become mandatory in order to prevent future human health implications.
We have found that implementing our proposal will actually be met with success and support from society. Walking around a grocery store today you can easily spot a growing number of labels claiming “antibiotic free” meat. For instance, Whole Foods does not allow any meat in its store that is not from an antibiotic free farm (Gallo, 2012). On social media there are a growing number of articles spreading awareness about antibiotic resistance. This issue is becoming more well known each day and farms all over the country are realizing the growing demand and converting to be antibiotic free products. One farm in particular is Wayne Farms. Most people associate becoming antibiotic free with small farms, however Wayne Farms is the 6th largest poultry producer in the United States (Wayne Farms, 2016). They sell 2.6 million pounds of chicken every year and believe that raising a happy, healthy bird while also protecting the environment is a very important part of farming (Wayne Farms, 2016).
With that said, we do understand that the ban of antibiotics for sub therapeutic and non-therapeutic purposes will have an economic impact on meat production and sales. The practice of antibiotic overuse has resulted in animals weighing more at the time of slaughter. Typically, cattle raised with antibiotics are ready for market in 16 months, while antibiotic free cattle do not leave for slaughter until 20 months old (Gallo, 2012). This means farmers need to pay for 4 extra months of feed and care for their livestock. Antibiotic raised livestock appear to stay healthier for the duration of their growth time which is a major benefit to farmers (Rummo, 2016). There is arguably an important role of antibiotics in making profitable and efficient production of livestock meat (Chattopadhyay, 2014).
However, as time goes on antibiotic resistance is only growing and will soon become a human epidemic and cost taxpayers thousands of dollars to compensate for a growing number of antibiotic resistant infections (Walsh, 2014). The total economic burden placed on the U.S. economy by antibiotic-resistant infections have been estimated to be as high as $20 billion in health care costs (Ventola, 2015, para. 47). These infections also burden families and communities due to lost wages and lost productivity (Ventola, 2015). There is an estimated medical cost per patient with an antibiotic resistant infection ranging from $18,588 to $29,069 depending on severity (Bartlett, Gilbert, & Spellberg, 2013, p.1446). These numbers will only grow as antibiotic uses increases (Bartlett, 2013). Consumers have started paying attention to this issue, too. The USDA reported that the sale of food labeled organic have risen from $11 billion in 2004 to approximately $32 billion in 2013 (Sneering et al., 2015, p.58). Even fast food chains like McDonald’s, Chipotle, and Panera bread now have antibiotic free chicken and beef (McKerrow, 2012). As more restaurants and grocery stores demand antibiotic free meats, more pressure is going to put on farmers to produce. As for the claim that antibiotic fed livestock keeps animals healthier and happier, this may appear true on the surface, but in reality farms with antibiotic free livestock need to be more attentive to their animals and catch any potential health problems before they spread. Farms with antibiotics do not constantly check the health and welfare of their animals so, if an animal does get sick, it will spread to most of the antimicrobial resistance herd before being noticed (Gallo, 2012). Antibiotic free farms have found that their animals’ overall welfare and health actually improved (Wayne Farms, 2016).
As the trend for antibiotic free meat grows, consumers are becoming increasingly aware of the various risks antibiotic resistant bacteria pose to human health. Antibiotics have been overused to an extreme in order to promote growth and health in livestock animals. This overuse has caused a mass production of antibiotic resistant bacteria to develop. The lack of regulation on antibiotic use in CAFOs has led to surface and groundwater contamination. These contaminations impact the future health of humans as we will have no way to combat the antibiotic resistant bacteria. Given these problems, we propose that the use of non-therapeutic and subtherapeutic antibiotics be eliminated entirely from livestock production. Although this will raise meat prices somewhat, the increase in taxes and medical bills will surely be even more impactful. Also, societal pressures for farms to conform to be antibiotic free are rising due to consumer demand. It will become essential for farms to convert in order to stay in business. Research has shown how important it is that the use of non-therapeutic and subtherapeutic antibiotics in our livestock must be diminished in the future to prevent a widespread human epidemic (Walsh, 2014).
Reference List:
Antimicrobial Resistance Learning Site. (2011). Growth Promotion. Retrieved from: http://amrls.cvm.msu.edu/pharmacology/antimicrobial-usage-in-animals/non-therapuetic-use-of-antimicrobials-in-animals/use-of-antibiotics-in-animals-for-growth-promotion
Bartlett, G., Gilbert, D., & Spellberg, B. (2013) Seven ways to preserve the miracle of antibiotics. Oxford Journals. 56(10). Retrieved from: http://cid.oxfordjournals.org/content/56/10/1445.long
Beecher, C. (2015). Managing “Black-Gold”: Animal Manure and Antibiotic Resistance. Food Safety News. Retrieved from: http://www.foodsafetynews.com/2015/11/managing-black-gold-animal-manure-and-antibiotic-resistance/#.WCO8Lckn72t
Brooks, C. (2011). Meat’s environmental impact. Stanford Woods: Institute for the Environment.
URL: https://woods.stanford.edu/news-events/news/meats-environmental-impact
Chattopayhyay, M.K. (2014). Use of antibiotics as feed additives: a burning question. Frontiers
of Microbiology. Doi: 10.3389/fmicb.2014.00334
Clark, S., R. Daly, E. Jordan, J. Lee, A. Mathew, and P. Ebner. 2012. Extension Education Symposium: The future of biosecurity and antimicrobial use in livestock production in the United States and the role of extension1. J. Anim. Sci. 90:2861-2872. doi:10.2527/jas.2011-4739
Dolliver, H., Kumar, K., & Gupta, S. (2007). Sulfamethazine Uptake by Plants from
Manure-Amended Soil. Journal of Environmental Quality, 36, 1224-1230. Doi:
10.2134/jeq2006.0266
Editorial Board. (2013). The antibiotic resistant crisis. The New York Times. Retrieved
from: http://www.nytimes.com/2013/09/18/opinion/the-antibiotic-resistance-crisis.html
Environmental Protection Agency. (2016). Animal Feeding Operation. Retrieved from
https://www.epa.gov/npdes/animal-feeding-operations-afos
Environmental Protection Agency. (2004). Water on tap: A consumer’s guide to the nation’s drinking water. Retrieved from http://permanent.access.gpo.gov/lps21800/www.epa.gov/safewater/wot/ wheredoes.html
Environmental Protection Agency. (1998). Environmental impacts of animal feeding operations. Retrieved from http://www.epa.gov/waterscience/guide/feedlots/envimpct.pdf
Environmental Protection Agency. (2016). Animal Feeding Operation. Retrieved from
https://www.epa.gov/npdes/animal-feeding-operations-afos
Environmental Protection Agency. (2016). Animal Feeding Operation. Retrieved from
https://www.epa.gov/npdes/animal-feeding-operations-afos
Food and Drug Administration. (2015). FDA’s strategy on antimicrobial resistance-questions and answers. Retreived from: http://www.fda.gov/animalveterinary/guidancecomplianceenforcement/guidanceforindustry/ucm216939.htm
Gallo, A.C. (2012). Our meat: no antibiotics ever. Whole Foods Market. Retrieved from: http://www.wholefoodsmarket.com/blog/whole-story/our-meat-no-antibiotics-ever-0
Hays, V.W. 1991. “Effects of antibiotics.” In: Growth Regulation in Farm Animals. Advances in Meat Research. Vol. 7. A.M. Pearson and T.R. Dutson, eds. Pp. 299-320. New York: Elsevier Applied Science.
Kaufman, M. (2000). Worries rise over effect of antibiotics in animal feed; Humans seen vulnerable to drug-resistant germs. Washington Post, p. A01. Retrieved from http://www.upc-online. org/000317wpost_animal_feed.html
Mackie, R.I., Maxwel, S., Aminov, R.I., Chee-Sanford, J., Koike, S., & Krapac, I., (2006). Animal Biotechnology, 17 (2), 157-176 URL: http://dx.doi.org/10.1080/10495390600956953; http://hdl.handle.net/10113/27530
McKerrow, K. (2012). The best way to play the antibiotic free meat trend. The Street. Retrieved from: https://www.thestreet.com/story/13746395/1/the-best-way-to-play-the-antibiotic-free-meat-trend.html
Mercola. (2015). CAFOs, your gut, and mental health. Retreived from: http://articles.mercola.com/sites/articles/archive/2015/03/25/cafos-gut-mental-health.aspx
Merriam-Webster Dictionary (2016). therapeutic. Retrieved from: http://www.merriam-
webster.com/dictionary/therapeutic
Passel, J.S. and Cohn, D. (2008). U.S. population projection: 2005-2050. Pew Research Center Retrieved from: www.pewsocialtrends.org/2008/02/11/us-population-projections-2005-2050/
Rummo, G. (2016). How feasible is antibiotic-free meat? Beef. Retrieved from: http://beefmagazine.com/beef-quality/how-feasible-antibiotic-free-meat
Sapkota, A. R., Curriero, F. C., Gibson, K. E., & Schwab K. J. (2007). Antibiotic-resistant enterococci and fecal indicators in surface water and groundwater impacted by a concentrated swine feeding operation. Environmental Health Perspectives, 115(7), 1040-1045. Doi:10.1289/ehp.9770
Sneeringer, S., MacDonald, J., Key, N., McBride, W., & Mathews, K. (2015) Economics of antibiotic use in U.S. livestock production. Department of Agriculture,Economic Research Service
South Dakota State University. (2016). Antibiotics in cattle. Retrieved from:
http://www.sdstate.edu/beef-procedures-antibiotic-use
U.S. Food and Drug Administration. (2016). FDA’s strategy on antimicrobial resistance. Retreived from: http://www.fda.gov/animalveterinary/guidancecomplianceenforcement/guidanceforindustry/ucm216939.htm
United States Department of Agriculture. (2014) Antimicrobial Resistance. Retrieved from:
http://www.usda.gov/documents/usda-antimicrobial-resistance-action-plan.pdf
United States Department of Agriculture. (2015) Production Purposes. Retrieved from: https://www.ers.usda.gov/amber-waves/2015/november/restrictions-on-antibiotic-use-for-production-purposes-in-us-livestock-industries-likely-to-have-small-effects-on-prices-and-quantities/
United States Geologic Survey. (1993) The World’s Water. Retrieved from:
http://water.usgs.gov/edu/earthwherewater.html
Ventola, C. (2015). The antibiotic resistance crisis. US National Library of Medicine National
Institutes of Health, 40(4), p. 277-283.
Walsh, F. (2014). Superbugs to kill ‘more than cancer’ by 2050. BBC. Retrieved from: http://www.bbc.com/news/health-30416844
Wayne Farms. (2016). Our facilities. Retreived from: http://waynefarms.com/facilities
West, B., Liggit, P., Clemans, D., & Francoeur, S. (2011). Antibiotic resistance, gene transfer, and water quality patterns observed in waterways near CAFO farms and wastewater
treatment facilities. Water, Air, & Soil Pollution, 217(1), 473-489.
doi:10.1007/s11270-010-0602-y
Zeller, B. (2016). AHI statement on FDA final rule of antibiotic sales estimates. Animal Health Institute. Retrieved from: http://www.ahi.org/archives/2016/05/ahi-statement-fda-final-rule-antibiotic-sales-estimates/
http://www.veganoutreach.org/whyvegan/images/lagoon.jpg
http://www.iflscience.com/health-and-medicine/manure-antibiotic-free-cows-still-contributing-resistance/
I think we should use antibiotics, if it is very necessary. We should give our body to deal with minor ailments and try to boost our body to make it more healthy. The yoga can also be useful for treating long term body illness.
You may find this study relevant in this regard with title “Role of Yoga in Ancient Menstrual Ethics with special reference to concept of Citta Suddhi†published in Praxis International Journal of Social Science and Literature, Vol. 4, Issue 7, URL ww.pijssl.com, DOI:
Best counseling before treatment, precise study of the problem, strictly Ayurveda-based medication, personalized and affordable treatment packages, and sexologist in Delhi fulfill all the categories that an ideal sexologist treatment in Delhi requires.
I will recommend your website to everyone. You have a very good gloss. Write more high-quality articles. I support you, indian matka
I like this article about the effect of antibiotic use on livestock, animals groundwater, and humans, thanks for sharing this helpful info
Ravi Gupta SEO Expert is The Place For Next-Level SEO And Link Building Strategies. We Cover About Search Engine Optimization
Antibiotics are used to treat or prevent some types of bacterial infection and prescribed in health problems. Its usage can be like a double-edged sword. The use of antibiotics must be very careful to secure your future. This article will provide you information on why and how to use Antibiotics precisely. Read Now…
Visit: https://bit.ly/32YOSKu
Its helpful post.
Great read! I had no idea about the smog in China containing antibiotic-resistant genes, how interesting and alarming. I too am doing a similar study on how antibiotic use in animals is contributing to the resistant bacteria issue, I was surprised to find that 80 per cent of antibiotics sold in the U.S. are given to farm animals and these meds go further than the animals. They are also impacting us environmentally in our water and soil. Stricter regulations on appropriately using antibiotics in animals, for example, to treat sickness only, would be a step in the right direction.
martini shaker set
I think we should use antibiotics, if it is very necessary. We should give our body to deal with minor ailments and try to boost our body to make it more healthy. The yoga can also be useful for treating long term body illness.
You may find this study relevant in this regard with title “Role of Yoga in Ancient Menstrual Ethics with special reference to concept of Citta Suddhi” published in Praxis International Journal of Social Science and Literature, Vol. 4, Issue 7, URL ww.pijssl.com, DOI: 10.51879/pijssl/040705
online income source