As we reach the end of a year in which the world has suffered through the worst respiratory-disease pandemic in a century, it is natural that we look ahead and wonder what we should expect for the coming year. Speculation about the timeline for a “return to normal” began as early as April, when the pandemic had just begun to unfold in Europe and North America. Nine months later, it is increasingly a topic of discussion both in the public sphere and in casual conversations amongst friends and neighbors. One of the more striking aspects of this discourse is how persistently gloomy it remains in many corners, despite the mounting evidence that augurs a relatively quick return to the vibrant, healthy society that existed before the pandemic. Much of this pessimism can be attributed to the ever-present reminders of the most frightening aspects of the pandemic – the COVID dashboards and graphics, the steady drumbeat of reporting of death milestones, the comparisons of the death toll to that of terrorist attacks – and the sensationalist reporting of outcomes that are exceedingly rare and, often, only very tenuously attributable to COVID (Kawasaki-like disease in children[1], teeth falling out[2], erectile disfunction[3], psychoses[4]). All the while, positive signs are typically shrouded in a cloud of caveats and qualifying statements that cast doubt on the reliability of the information. Over time, this has solidified into a standard narrative that has proved remarkably difficult to counter. The end result is a populace increasingly pushed to the limits of COVID fatigue, left wondering if society will ever regain its footing.
Early in 2020, experts spoke of an effective end of the pandemic and return to a “new normal” in late 2021, at the earliest, with the arrival of an effective vaccine coming too late to make a significant difference in the overall timeline.
“we must be prepared for at least another 18 to 24 months of significant Covid-19 activity, with hot spots popping up periodically in diverse geographic areas…So, lacking a vaccine, our pandemic state of mind may persist well into 2021 or 2022…”
https://www.nytimes.com/2020/05/08/health/coronavirus-pandemic-curve-scenarios.html (“This Is the Future of the Pandemic,” Siohban Roberts, 8 May, 2020)
This set the baseline for expectations: a pandemic, with its concomitant non-pharmaceutical interventions (NPI), consisting of lockdowns, social distancing and other suppression efforts, that will span a miserably long period of 18 to 24 months.
As we entered the Fall, however, the first glimmers of hope for a more rapid escape from the nightmare were emerging: early results from several vaccine trials were promising, and timelines indicated that millions of doses could be ready for distribution to the population as early as the end of the year. Not to be deterred, the reflexive posture of the media was to temper expectations and frustrate any nascent effort to begin seeing the light at the end of the tunnel!
“Americans are also overestimating what a vaccine might do. Many are focusing on whether approval is being rushed as a campaign ploy, but that’s almost beside the point. It seems likely that a vaccine will be approved this fall and that it will be ‘effective.’ But it’s very unlikely that this vaccine will be a game changer…We don’t know yet where a coronavirus vaccine will fall, although something along the lines of a flu shot seems more probable. We don’t know how long whatever immunity it provides will last. We don’t know whether there will be populations that derive more or less benefit…Even this assumes, of course, that we can distribute the vaccine widely and quickly (which is doubtful), that most people will get it (many won’t) and that we will succeed in prioritizing distribution so that those most at risk will get it first (flying in the face of decades of disparities in the way health care is distributed).”
https://www.nytimes.com/2020/09/15/opinion/coronavirus-precautions.html (“Stop Expecting Life to Go Back to Normal Next Year,” Aaron Carroll, 15 Sep., 2020)
In November, many of these unknowns evaporated, when efficacy and safety results for the Pfizer and Moderna vaccines were finally released: efficacies of around 95%, far surpassing expectations, and no reported serious adverse effects in the more than 20,000 individuals who participated in the vaccinated arm of each of the trials.
“’This is really a spectacular number,’ said Akiko Iwasaki, an immunologist at Yale University. ‘I wasn’t expecting it to be this high. I was preparing myself for something like 55 percent.’”
https://www.nytimes.com/2020/11/09/health/covid-vaccine-pfizer.html (“Pfizer’s Early Data Shows Its Vaccine is More Than 90% Effective,” Katie Thomas, David Gelles, Carl Zimmer, 9 Nov., 2020)
“The drug maker Pfizer said on Wednesday that its coronavirus vaccine was 95 percent effective and had no serious side effects…The data showed that the vaccine prevented mild and severe forms of COVID-19, the company said. And it was 94 percent effective in older adults, who are more vulnerable to developing severe Covid-19 and who do not respond strongly to some types of vaccines.”
https://www.nytimes.com/2020/11/18/health/pfizer-covid-vaccine.html (“New Pfizer Results: Coronavirus Vaccine is Safe and 95% Effective,” Katie Thomas, 18 Nov., 2020)
Surely with a vaccine of spectacularly high efficacy presently in deployment, Americans could now begin to entertain some degree of hope that life would return to normal on an appreciably shorter timeline than previously imagined? Not so fast, we are told. While a “minority” of the experts believe this possible, the consensus is, strangely, as pessimistic as ever – no change in the baseline!
“A minority of the epidemiologists said that if highly effective vaccines were widely distributed, it would be safe for Americans to begin living more freely this summer: ‘I am optimistic that the encouraging vaccine results mean we’ll be back on track by or during summer 2021,’ said Kelly Strutz, an assistant professor at Michigan State University…But epidemiologists are a very cautious group. Most said that even with vaccines, it would probably take a year or more for many activities to safely restart, and that some parts of their lives may never return to the way they were. Karin Michels, professor of epidemiology at U.C.L.A., said it would probably be many years until it was safe enough to ‘return to approximately the lifestyle we had.’ She said, ‘We have to settle to live with the virus.’”
https://www.nytimes.com/2020/12/04/upshot/epidemiologists-virus-survey-.html (“How 700 Epidemiologists are Living Now, and What They Think is Next,” 4 Dec., 2020)
This mostly-unidentified panel of 700 experts are indeed some of the most cautious members of the population. According to the article, 74% had yet to send their children on an outdoor playdate, 38% had not yet “hiked or gathered outdoors with friends,” 28% still were not “bringing in mail without precautions,” and 10% had not even “gone on errands, such as to the grocery store or the pharmacy.” Little wonder, then, that they foresee such a long, possibly never-ending road to the pre-COVID life many of us are already forgetting had ever existed.
Even Dr. Anthony Fauci, America’s most respected expert in infectious diseases, is apt to keep us off balance – grateful for the unprecedented speed in which highly-effective vaccines have been developed and brought to market, while all the same quietly ‘moving the goal posts.’
“Recently, a figure to whom millions of Americans look for guidance — Dr. Anthony S. Fauci, an adviser to both the Trump administration and the incoming Biden administration — has begun incrementally raising his herd-immunity estimate…In a telephone interview the next day, Dr. Fauci acknowledged that he had slowly but deliberately been moving the goal posts. He is doing so, he said, partly based on new science, and partly on his gut feeling that the country is finally ready to hear what he really thinks…”
https://www.nytimes.com/2020/12/24/world/how-much-herd-immunity-is-enough.html (“How Much Herd Immunity is Enough?” Donald McNeil, 24 Dec., 2020)
Does any of this make sense? The myriad deleterious effects from NPIs being just as serious as COVID itself, should we not strive to end them on as hasty a timeline as reasonably possible?
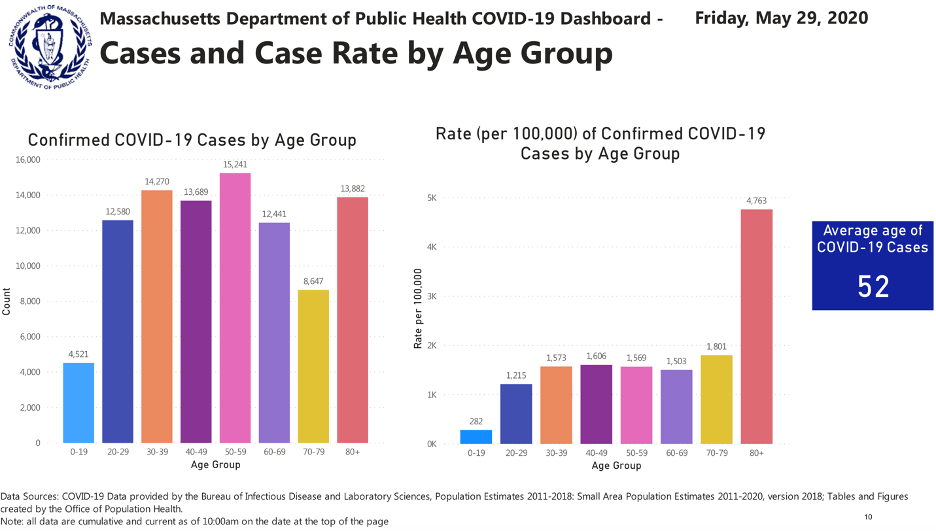
If we make a reasonable appraisal of the situation in the US, and put aside any biases we may have due to ‘gut feelings,’ the forecast for 2021 is decidedly more positive than most seem to realize. The distinguishing feature of the pandemic is the relatively high rate of hospitalizations and deaths attributable to COVID in the elderly population, and it is in this population that a successful vaccination campaign will be paramount. Nursing home residents make up a dramatically disproportionate share of COVID deaths. They represent less than 1% of the US population (about 2.5 million, in all), but so far account for more than 38% of all COVID deaths (https://covidtracking.com/data/long-term-care) – and in some states, the figure is much higher (in Massachusetts, it stands at 60%). More than one million Americans have already received the first dose of the vaccine, and by the middle or end of January we can expect that all residents and workers in nursing homes will have been vaccinated; in the Massachusetts schedule (https://www.mass.gov/info-details/when-can-i-get-the-covid-19-vaccine), this group is second highest in priority amongst the six groups covered by Phase 1 of the campaign, where the projected timeline is December 2020 – February 2021. The next-most at-risk demographic is elderly Americans living in the community (outside of care homes): persons over 70 years old, about 15% of the population, account for 80% of COVID deaths (https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm) A credible estimate for when this group will have been fully vaccinated is the end of March or April (Phase 2 in the Massachusetts plan). The Pfizer and Moderna vaccines have been shown to work nearly equally well in the elderly population as they do in in the younger population, and they reduce Sars-Cov-2 infections that present as mild to moderate symptoms by a factor of twenty. There were zero cases of severe symptoms and zero deaths in the vaccinated groups, signifying protection against severe forms of COVID very close to 100%. It follows that hospitalizations and deaths due to COVID will steadily fall through the Winter, as the most at-risk members of the population become inoculated. As an example, the daily rate of COVID deaths in the population over 70 would be reduced, via vaccination, from its current value of about 1,800 (nearly its highest value since the pandemic began) to less than 90!
But the fraction of the population that is vaccinated does not tell the whole story – there are also the tens of millions of Americans who have acquired durable immunity through infection by the virus itself. Many seem to believe, having been influenced by early, misleading media reports regarding waning antibody levels, that immunity is either very fleeting or even on-existent. The truth of the matter is that reports of reinfection remain vanishingly small and all evidence points to long-lasting immunity – likely a year or two, possibly even longer.
“Within the last couple of months, several scientific studies have come out — some peer-reviewed, others not — indicating that the antibody response of people infected with SARS-CoV-2 dropped significantly within two months. The news has sparked fears that the very immunity of patients with Covid-19 may be waning fast — dampening hopes for the development of an effective and durable vaccine.
But these concerns are confused and mistaken…”
(“Scared That COVID-19 Immunity Won’t Last? Don’t Be,” Akiko Iwasaki and Rusian Medzhitov, 31 July, 2020)
“How long might immunity to the coronavirus last? Years, maybe even decades, according to a new study.”
https://www.nytimes.com/2020/11/17/health/coronavirus-immunity.html (“Immunity to the Coronavirus May Last Years, New Data Hint,” Apoorva Mandavilli, 17 Nov., 2020)
The CDC estimates that by the end of November 2020 about 91 million Americans had already been infected (https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/burden.html, https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa1780/6000389). Using the same model parameters, it is conceivable that around 120 million, more than a third of the US population, will have been infected by the end of December. Unlike in the earliest phase of the epidemic, younger Americans (< 50 years of age) are now the majority of those being infected. Combining this large population of younger Americans who have acquired immunity naturally with the vaccinated population, which will initially skew towards older Americans, the full population-wide, or herd, immunity will already be very substantial by mid-Spring 2021, when the vaccine becomes available to the general population (Phase 3 in the MA plan). The growth of herd immunity through the Winter and Spring will drive hospitalizations and deaths in the under 70 segment of the population to progressively lower levels, even before accounting for the effects of vaccination in this same group.
A likely scenario is that by Summer 2021 COVID will have ceased to be a serious public health threat and Americans of all ages will be leading normal lives, unburdened by the demands of social distancing. The restaurant, hospitality, tourism and cultural event sectors of the economy will finally emerge from the devastation wrought by the pandemic and we will be on the road to full economic recovery. Such is the story of every pandemic of the last 100 years (Fig. 1), and there is absolutely no reason to believe that this one is any different.
“According to historians, pandemics typically have two types of endings: the medical, which occurs when the incidence and death rates plummet, and the social, when the epidemic of fear about the disease wanes.”
https://www.nytimes.com/2020/05/10/us/coronavirus-deaths-cases.html (“When Will the Pandemic End? And How?” 10 May, 2020)
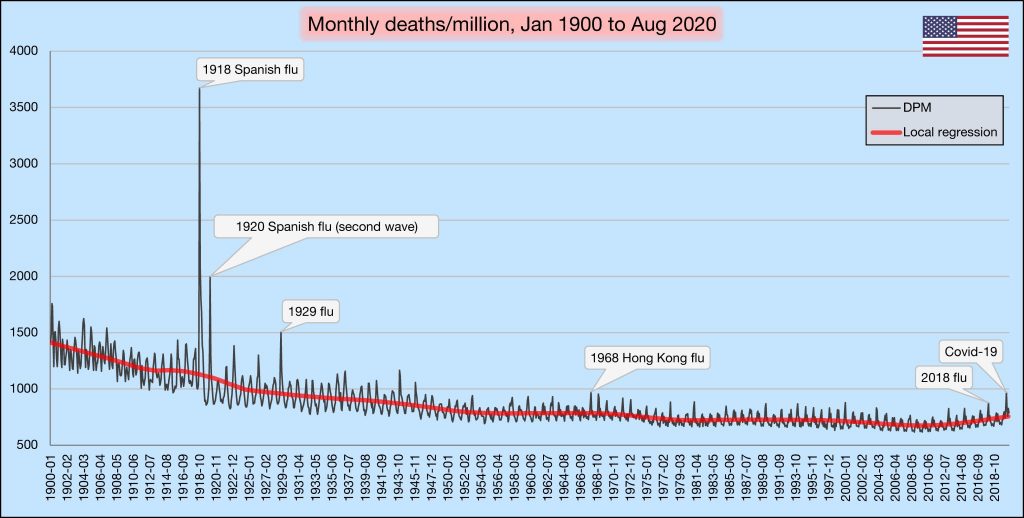
Figure 1: Number of deaths (all-cause) per month, per million inhabitants, Jan. 1900 – 1 Sep. 2020, as recorded by the US CDC. Notable respiratory-disease pandemics are indicated (most other peaks are seasonal, non-pandemic influenza deaths). N.B. The graph includes data through the end of Aug. 2020, when Covid-19 deaths tallied 188,000 – there is a second peak of an additional 140,000 total deaths in the final four months of the year (106 deaths per month, per million). Credit: @VoidSurf1 (Twitter Handle), from public CDC data (https://www.cdc.gov/nchs/nvss/mortality/hist293.htm
Carlo Dallapiccola (carlo.dallapiccola@gmail.com)
Thanks to Rosie Cowell, Dave Huber and Adrian Staub for helpful discussion and comments.
[1] https://www.washingtonpost.com/health/2020/05/05/coronavirus-children-kawasaki-syndrome/ “15 children in New York City have developed a puzzling and serious inflammatory syndrome possibly linked to covid-19,” 5 May, 2020.
[2] https://www.nytimes.com/2020/11/26/health/covid-teeth-falling-out.html “Their Teeth Fell Out. Was It Another Covid-19 Consequence?” 28 Nov., 2020.
[3] https://www.nytimes.com/2020/06/04/smarter-living/the-pandemic-is-stressing-your-body-in-new-ways.html “The Pandemic Is Stressing Your Body In New Ways,” 4 June, 2020.
[4]https://www.nytimes.com/2020/12/28/health/covid-psychosis-mental.html “Small Number of Covid Patients Develop Severe Psychotic Symptoms,” 28 Dec., 2020.